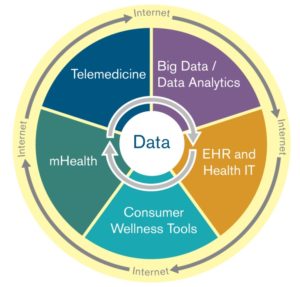
Digital health—the intersection of health care related software applications, analytical tools, medical device technology and electronic data assets that are enabled and achieved through the use of the internet and hand-held devices—is empowering the innovation needed to meet the imperative for a transition from payment based on volume to payment based on value that is evaluated in terms of measurable improvements in care delivery and population health.
One prominent example is the use of digital health solutions to implement the payment innovation contemplated by the Medicare Access and CHIP Reauthorization Act (known as MACRA)—which directly ties both payment increases and reductions to various, specific efficiency and value measures. The Merit-Based Incentive Payment System (MIPS), one of the two available payment pathways under MACRA, assigns points to clinicians in different performance categories, several of which promote the adoption of digital health solutions. To illustrate:
- The Quality category requires six measures to be reported, many of which may be leveraged through the use of digital health tools. For example, the Maternity Care: Post-Partum Follow-Up and Care Coordination measure tracks the percentage of patients who were seen for post-partum care within eight weeks of giving birth who received particular evaluations, screening and education. Obstetricians, gynecologists and family medicine practitioners could earn points under this measure by using telemedicine technologies, like videoconferencing platform, to engage in virtual patient visits with post-partum patients to answer the patient’s questions, provide education on the recovery process and assess the patient’s physical and mental health status, including the performance of mandatory post-partum depression screenings.
- The Advancing Care Information category requires the use of certified electronic health record technology to coordinate care through patient engagement (g., secure messaging). The implementation of patient portals with integrated messaging platforms facilitate communication between the patient and health care practitioner, providing additional functionalities like sending reminders, engaging in dialogue about follow-up care, encouraging preventative action and distributing educational materials. These portals typically also give the patient access to timely and informative data, like test results, that allow the patient to play a role in decision making and (hopefully) empower the well-informed consumption of care.
- The Clinical Practice Improvement category is perhaps the best opportunity for digital health integration. Activities that improve beneficiary engagement, population management, expanded practice access and care coordination—among others—are assigned points and weighted. Here, mobile apps have the capability to enable e-visits via videoconference as an alternative method to an in-person visit; facilitate questionnaire reporting; and send reminders, materials and other notifications to alert and educate patients about services due. The apps also provide opportunities to generally inform the delivery of care for the specific patient by sending alerts to providers to indicate that it’s time for a visit or that a problematic symptom was noted on a questionnaire. Further, clinical practices could leverage app-sourced data to gain information about patient trends, clinical areas of concern or successes related to digital health tool utilization.
For [...]
Continue Reading
read more

 Subscribe
Subscribe