In 2017, the New Jersey legislature passed the New Jersey Telehealth and Telemedicine Act (codified at N.J.S.A. 45:1-61 et seq.), which established registration and reporting requirements for “telemedicine and telehealth organizations.” After a multi-year wait for details regarding the registration process, the New Jersey Department of Health (NJ DOH) published a proposed rule in April 2020 that brought providers of telehealth services in New Jersey one step closer to the implementation and enforcement of the registration requirements. A final rule is expected by April 2021.
New Jersey providers are also expecting the publication of a proposed rule detailing the reporting requirements for registered organizations. While the coronavirus (COVID-19) public health emergency has led many states to implement waivers and other measures to allow for the expansion of remote healthcare services within their states, telehealth and telemedicine organizations operating in New Jersey should prepare to comply with additional requirements and the outlay of annual registration fees if the state finalizes the registration requirements as proposed.
Background: The 2017 Telemedicine and Telehealth Act
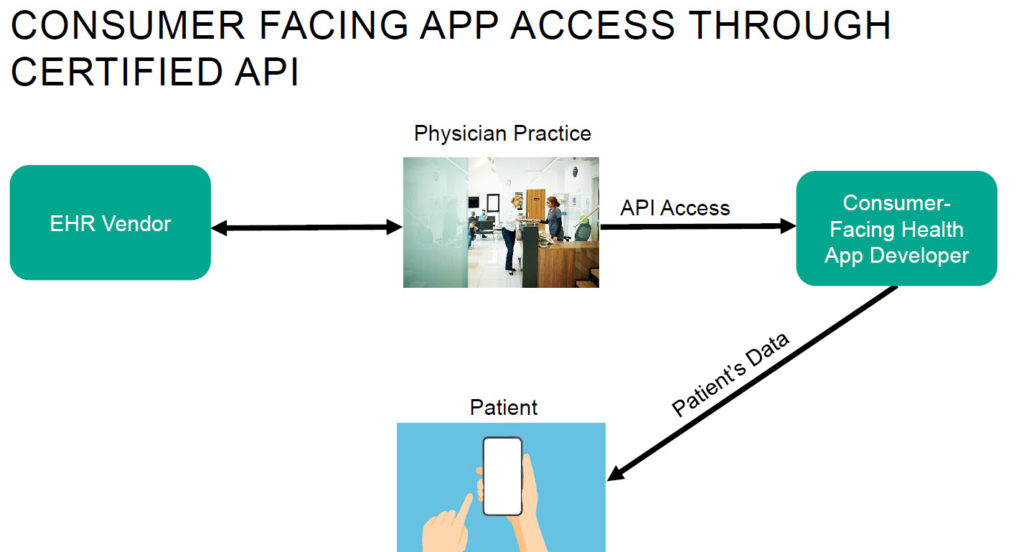
For purposes of the Act, a “telemedicine or telehealth organization” is defined as a corporate entity “that is organized for the primary purpose of administering services in furtherance of telemedicine or telehealth.” The Act differentiates telemedicine from telehealth: “telehealth” is the use of information and communications technologies (including telephones, remote patient monitoring devices or other electronic means) to support clinical healthcare, provider consultation, patient and professional health-related education, public health, health administration and other services, whereas “telemedicine” is the delivery of healthcare services using electronic or technological means (not including the use, in isolation, of audio-only telephone, electronic mail, instant messaging, phone text or facsimile transmission) to “bridge the gap” between a healthcare provider located at a distant site and a patient located at an originating site.
In addition to establishing requirements for providers’ use of telemedicine and telehealth, the Act requires telemedicine or telehealth organizations to register with the NJ DOH annually, and to submit annual reports to the NJ DOH that include data elements established by the NJ DOH commissioner and, at a minimum, the following de-identified encounter data:
- The total number of telemedicine and telehealth encounters conducted
- The type of technology utilized to provide services using telemedicine or telehealth
- The category of medical condition for which services were sought
- The geographic region of the patient and the provider
- The patient’s age and sex
- Any prescriptions issued.
The Act did not establish any enforcement mechanism for the registration and reporting requirements, and because the NJ DOH has not yet implemented criteria for registering or reporting, New Jersey providers of remote health services have generally operated without regard to these statutory requirements.
Implementation of the Registration Requirement
The April 2020 proposed rule would implement the registration requirement for telemedicine or telehealth organizations and establish enforcement mechanisms available to the NJ DOH against any telemedicine or telehealth organization that fails to comply.
The proposed rule would require telemedicine and telehealth organizations to register with the NJ DOH [...]
Continue Reading
read more

 Subscribe
Subscribe